2024 Annual Texas NMDOH Consortium Conference: Advancing Research, Policy and Practice
December 5 – 6, 2024
Houston, Texas
Join the Texas NMDOH Consortium for our 2nd Annual Texas NMDOH Consortium conference. We have expanded to a two-day event exploring the latest developments in operations, regulation, and financing the integration of NMDOH interventions into healthcare delivery systems in Texas. This convening is an opportunity for health care providers, policymakers, and researchers to engage with fellow experts, share insights, and contribute to conversations to improve health care quality in Texas.
WHERE
Rice University Bioscience Research Collaborative
6500 Main Street
Houston, TX 77030
https://brc.rice.edu
This conference is co-sponsored by the founding members, Rice University’s Baker Institute for Public Policy, and UTHealth Houston’s Center for Health Care Data.


2024 NMDOH Conference Presentation Slides
Main Conference
Post-Election Federal Landscape for NMDOH Policy
Sustaining Food is Medicine Programs in Texas
What to Expect in the 89th Legislative Session
Working With Managed Care Organizations to Integrate NMDOH
Breakout Sessions
The Experience of Non-Profit Hospitals in Responding to Patients’ Non-Medical Needs
Using Risk Stratification to Identify and Address NMDOH Needs in Rural Communities
Shared Medical Appointments: An Interdisciplinary Pathway to Reimbursement for NMDOH Services
Building Capacity for NMDOH Integration through Research Partnerships
Practical Strategies for NMDOH Screening and Resource Delivery in Complex Populations
2024 Conference Agenda
2024 Texas NMDOH Consortium Conference Speakers

Dr. Alexandra Jones Adesina, Chief Equity Officer, Waco Family Medicine
Shared Medical Appointments: An Interdisciplinary Pathway to Reimbursement for NMDOH Services
Dr. Jones Adesina is the inaugural Chief Equity Officer at Waco Family Medicine, whose primary role is to set the vision of equitable health care delivery by managing programs that address social drivers of health, maternal health outcomes, and staff equity initiatives. Her ongoing vision is to make transformational systems change to eliminate health outcome disparities while caring for patients throughout their lives.
A Waco native, Dr. Jones Adesina practices family medicine after spending time in Chicago, where she taught with Teach [F]or America before starting medical and public health school at Northwestern University Feinberg School of Medicine and then completing a family medicine residency in Lancaster, Pennsylvania. Dr. Jones Adesina leverages her insights and experiences in providing patient care to inform equity initiatives.
In her spare time, Dr. Jones Adesina enjoys time with her family, reading, cooking, and traveling. Most recently, she enjoyed a magical trip to Paris for the Summer 2024 Olympics.

Ashley Allison, Executive Director, Waco Foundation
Philanthropy’s View of NMDOH
Ashley Allison is the Executive Director of Waco Foundation, where she manages all aspects of a $150 million community foundation with the mission of improving the quality of life in McLennan County.
Ashley obtained her Bachelor of Arts in Economics at Baylor University and a Master of Arts in Political Science from West Texas A&M University. During her early career, she worked at a Council of Governments, writing grants for public infrastructure projects through the Texas Department of Housing and Community Affairs. Since 1994, she has worked in the community foundation field, including service with Amarillo Area Foundation, where she left as Vice President and two community foundations in the Boston area, where she was President & CEO. She has been the executive of the Waco Foundation for the past 17 years. During her career, she has raised over $30 million in grants and contributions for various community foundation efforts.
Ashley sits on the Steering Committee of the Groundwater Network, a national organization focused on advancing racial equity. She has also served nationally as faculty for the Council on Foundations Community Foundation Fundamentals Course, and she is a regular speaker at philanthropic conferences. As a part of the Leadership Council of Philanthropy Advocates, she is regularly involved in advocacy work related to Texas education policy. Locally, she is a member of the Waco Business League and Waco Leadership Forum. Ashley is a graduate of Leadership Waco (class of 2009) and Leadership Texas (2000).

Mital Brahmbhatt, System Director, Care Coordination & Population Health, Memorial Hermann
The Experience of Non-Profit Hospitals in Responding to Patients’ Non-Medical Needs
Mital Brahmbhatt brings nearly 20 years of experience in healthcare, where she has successfully developed and led programs focused on population health and care coordination. With a strong commitment to enhancing the healthcare journey, she has a track record of adding value through innovative strategies. Mital holds a Master of Social Work from the University of Houston and a Master of Healthcare Administration from Texas Woman’s University. Throughout her career, Mital has overseen operations in intensive care units, built a psychosocial division for the largest pediatric cancer center, and developed the STAR Kids Medicaid program for a health plan. She has worked to advance care coordination from payer to hospital to community, demonstrating its positive impact on patient care. Mital is passionate about being a change agent, both professionally and personally, dedicating her time to volunteer with three nonprofit organizations in the Houston area.
Currently, Mital serves as the System Director, Care Coordination & Population Health for Memorial Hermann’s Population Health Service Organization and is an adjunct professor at Texas Woman’s University. She is also an AHA NextGen Fellow for the 2024-2025 cohort.
Her teams focus on delivering comprehensive care coordination for approximately 400,000 ACO-attributed lives in the ambulatory space while driving innovative workflows in value-based care, case management, community coordination, HEDIS initiatives, and more. Mital’s purpose is to be an innovative, human-centered leader, advocating for patients, their families, and providers while striving to support those in need throughout their healthcare journey.

Arnita Burton, Associate Director, United HealthCare
Working With Managed Care Organizations to Integrate NMDOH
Arnita Burton is the Associate Director of Clinical Innovations, Analytics, and Non-Medical Drivers of Health at UnitedHealthcare Community Plan of Texas, the Medicaid division of UnitedHealth Group. This organization’s mission is to help people live healthier lives and help make the health system work better for everyone. Arnita has been with UnitedHealthcare for thirteen years, leveraging her extensive experience in healthcare operations management of government programs.
In her current position, Arnita oversees clinical initiatives and pilot programs implementing innovative strategies to improve traditional medical, behavioral, and pharmacy care management. These initiatives strongly emphasize addressing non-medical drivers of health, thereby delivering a comprehensive healthcare experience for diverse Medicaid populations and promoting health equity. Arnita is also engaged in UnitedHealthcare’s affordable housing projects, highlighting the valuable contributions in this area. A fulfilling part of Arnita’s role is facilitating collaboration among industry partners to advance critical healthcare policy and community initiatives.
Arnita holds a Doctorate in Healthcare Administration and a Master of Business Administration. Originally from Chicago, she has lived in Texas for over twenty years. In addition to her professional commitments, Arnita is actively involved in community service. She is a committed member of a local Women’s Empowerment Group, where she leads community projects, advocates for important causes, and supports professional development through mentorship programs.

Jill Campbell, Director of Community Benefits, Houston Methodist
The Experience of Non-Profit Hospitals in Responding to Patients’ Non-Medical Needs
Jill Campbell serves as the Director of Community Benefits at Houston Methodist where she manages external partnerships with community organizations and clinics through the department’s grants program, in-kind programs, charity care, and employee volunteerism. Within her role, she oversees implementation of strategies and grants programs directed toward increasing access to healthcare and mental health services, as well as programs addressing gaps in non-medical drivers of health in the region.
Prior to joining Houston Methodist, Jill most recently served as Director of Community Development and Engagement at BakerRipley, where she oversaw the agency’s youth, civic engagement, immigration, and citizenship programs and community centers. An immigration attorney by profession, from 2014-2023, she developed the organization’s immigration and citizenship program to respond to the region’s emerging immigration legal and social service needs. Jill has also served as a clinical supervising attorney at the University of Houston Law Center Immigration Clinic. In addition, Jill has served on multiple nonprofit boards and community councils, including the City of Houston Mayor’s Office of New Americans Advisory Committee, Casa Mateo, and Houston Immigration Legal Services Collaborative.

Andrew Cannon, Project Manager for Integrated Health, Burke
Using Risk Stratification to Identify and Address NMDOH Needs in Rural Communities
Andrew Cannon is currently the Project Manager for Integrated Health at Burke, where he manages the Nacogdoches Integrated Care Clinic and SUD Program. Previously, he worked as a Therapist for the Adult Mental Health program. He is a Licensed Professional Counselor and holds a Master of Arts in Clinical Mental Health Counseling and a Bachelor of Arts from Stephen F. Austin State University.

Dr. Cecilia Ganduglia Cazaban, Associate Professor, Director of the Center for Health Care Data, UT Health Houston School of Public Health
Opening Remarks
Dr. Ganduglia Cazaban is a medical doctor and an Associate Professor at UTHealth Houston School of Public Health. She is a highly trained health services researcher with extensive experience in the use of large administrative datasets for the evaluation of health care delivery, geographic variation in care processes, quality of care, and outcomes related to maternal and child health, chronic disease, and cardiovascular disease. She currently serves as the Director of the Center for Health Care Data (CHCD), the largest research-accessible data center in Texas. The CHCD houses national and Texas-based claims data, electronic health records data, and non-medical drivers of health. The Center has been named the All-Payor Claims Database for the state of Texas (HB2090 87th Legislative), which includes claims data for 80% of the insured population in Texas. Dr. Ganduglia Cazaban has authored numerous publications to evaluate the quality of care, geographic variation in care processes, non-medical health drivers, outcomes, and costs related to chronic disease as well as maternal and newborn care.

Dr. Shao-Chee Sim, Executive Vice President for Health Policy, Research and Strategic Partnerships, Episcopal Health Foundation
Philanthropy’s View of NMDOH
Dr. Sim is the Episcopal Health Foundation’s Executive Vice President for Health Policy, Research and Strategic Partnerships. Sim is also a nonresident fellow in health policy at Rice University’s Baker Institute for Public Policy and a member of HHSC’s Value-Based Payment and Quality Improvement Advisory Committee, where his work focuses on health policy and social determinants of health research. He currently leads the Foundation’s work in health coverage and health policy analysis, pilot projects, learning collaboratives, research, and evaluation portfolio. Current priorities include Medicaid managed care organizations’ social determinants of health (SDOH) strategies, multi-sectoral community health collaboratives, innovative SDOH financing strategies, community health center payment reform, rural healthcare service delivery, and public opinion survey research.
Dr. Sim currently serves on the Board of the Asian and Pacific Islander American Health Forum and National Rural Health Resource Center. He also serves on the Texas Health and Human Services Commission’s Value-Based Payment and Quality Improvement Advisory Committee.
His research has been published in health policy blog sites, including Health Affairs, Grantmakers in Health, Texas Medical Association, and Texas Primary Care Consortium; and peer-reviewed journals, including the Journal of Health Care for the Poor and Underserved, American Journal of Health Education, and Journal of American Board of Family Medicine.
He earned his Master’s degree in public administration from the JFK School of Government at Harvard University and a doctorate in public policy from the LBJ School of Public Affairs at the University of Texas at Austin.

Dr. Nancy Correa, Director of Population Health Strategy, Texas Children’s Hospital
The Experience of Non-Profit Hospitals in Responding to Patients’ Non-Medical Needs
Dr. Correa has dedicated her career to improving the lives of children and families. Dr. Correa is the Director of Population Health at Texas Children’s. In this role, she is responsible for developing and implementing a system-wide strategy for non-medical drivers of health and health equity. Dr. Correa has over fifteen years of experience in public health, and areas of focus include public health strategy, non-medical drivers of health, adverse childhood experiences, and early brain development. In 2020, Dr. Correa was the recipient of the Texas Pediatrics Society’s Distinguished Service Award, which is awarded to an individual for their contribution to improving the lives of Texas children. Dr. Correa has a bachelor’s degree from Rice University in Chemistry and Policy Studies, a master’s degree from Boston University School of Public Health, and a doctoral degree from the University of Texas School of Public Health.

Dr. Rakhi C. Dimino, Maternal Medical Director, Director of Midwifery Program, Houston Methodist
HB1575: Addressing the Non-Medical Needs of Pregnant and Postpartum Patients
Dr. Dimino has been delivering OB/GYN care to patients in Houston since 2006. She is passionate about continuous quality improvement, evidence-based care, and focusing on the individualized needs of each patient. She is the Maternal Medical Director for Houston Methodist Willowbrook and has worked to help implement patient safety bundles and improved protocols across the state of Texas. She started her career in private practice and then transitioned to providing emergency OBGYN care as an OBGYN hospitalist for 11 years. She has returned to private practice and enjoys teaching her patients as well as future generations of health care providers. Her undergraduate education was at Northwestern University in Evanston, IL. She attended medical school at The Ohio State University and completed her residency at Washington University in St. Louis. She has a Master’s in Medical Management from Carnegie Mellon University and is a Certified Physician Executive. She has served as Chair of the Board of Directors of the Preeclampsia Foundation and is a member of the Board of Directors for the Society of OB/GYN Hospitalists. She loves to volunteer at The Health Museum and is a member of their Board of Directors. She enjoys Scouting America with her son, volunteering at the Houston Food Bank with her daughter, and traveling with her husband and children.

Michelle Erwin, Deputy Associate Commissioner, Office of Policy, Medicaid and CHIP Services, Texas Health and Human Services
HB1575: Addressing the Non-Medical Needs of Pregnant and Postpartum Patients
Michelle Erwin leads the Medicaid and CHIP Services (MCS) Office of Policy as a Deputy Associate Commissioner at the Texas Health and Human Services Commission. The Office of Policy covers a range of policy functions, including medical and dental benefits policy development, program policy development, advisory committee support, and coordination with federal partners, and covers policy topics such as managed care, fee-for-service, acute care, long-term services, and supports, mental health, women’s health, etc. She has served in multiple roles in her 16 years with Texas Medicaid, including as a policy analyst, project manager, manager, and director. Michelle has a bachelor’s degree in Sociology and Writing from the University of Central Arkansas and a master’s degree in Sociology from Western Michigan University.

Michelle Fairley, Social Work Chronic Care Manager, Waco Family Medicine
Shared Medical Appointments: An Interdisciplinary Pathway to Reimbursement for NMDOH Services
Michelle Fairley is a Social Work Chronic Care Manager at Waco Family Medicine at two clinics, MLK and Elm Ave. Michelle is a 2-year breast cancer survivor, and going through the experience that I have endured has given me a different perspective and helped me be more understanding of the different health struggles that my clients are going through. I also have a great perspective on the challenges of getting healthcare needs taken care of for my clients’ health and well-being. She has a bachelor’s degree from Tarleton University and a master’s degree from UTA- Arlington. Michelle also has certificates in Mental Aid, Youth counseling and Mental Health/ Social worker.
Outside of work, Michelle enjoys spending time with her husband, Patrick Fairley of 27 years. Michelle also enjoys traveling, watching movies, shopping and enjoying quality time with her family.

Joshua Fernelius, Director of Population Health, Community Health Choice
Sustaining Food is Medicine in the Texas Landscape
Josh Ferneliusserves as the Director of Population Health at Community Health Choice (Community), a not-for-profit health plan in greater Houston that serves over 400,000 members across Medicaid, CHIP, Exchange, and a Medicare Dual-Special Needs Plan. He has over 10 years of experience in quality management, population health, and process optimization. He holds a Master of Public Health in Epidemiology from the University of Texas School of Public Health in Houston and two post-graduate certifications; a Certified Professional in Healthcare Quality from the National Association for Healthcare Quality and a Certified Lean Six Sigma black Belt from Villanova University. In his current role, he is responsible for enhancing the value of care delivery by developing strategies to improve health outcomes and address rising healthcare costs. His portfolio of work includes several community health worker initiatives aimed at building build trust and empowerment with members across the continuum of care as well as implementation support for a pathway for high-pregnant Medicaid beneficiaries to access the Houston Food Bank’s Food Rx Program.

Esperanza “Hope” Galvan PhD, MS, CVRN-BC, CDCES, Vice President Population Health, Harris Health
Building Capacity for NMDOH Integration through Research Partnerships
Esperanza “Hope” Galvan, PhD, MS, RN, CVRN-BC, CDCES, serves as the Vice President of Population Health Transformation at Harris Health, where she has served for over a decade in various leadership roles. In her current capacity, she successfully spearheaded the launch of the first cutting-edge, multi–sectoral clinic-based food prescription initiative for food insecure and diabetes patients in the region, which was recognized for innovation by American Essential Hospitals. She has oversight of remote patient monitoring, Patient Centered Medical Home accreditation, inpatient and outpatient patient educators, community health workers, and ambulatory clinic dietitians. In her current role, she continues to champion innovative solutions that address the root causes of health disparities, fostering healthier communities and promoting health justice.
As a board-certified cardiovascular nurse with over twenty-five years of experience, Hope holds extensive clinical experience in inpatient and outpatient nursing. She serves as a member of the American Association of Diabetes Educators (AADE), CDC and NIH National Diabetes Education Program (NDEP) Hispanic/Latino Stakeholder Group, Houston’s Health Equity Collective Steering Committee member, and Sigma Theta Tau International Honor Society of Nursing. She has also served in several advisory boards.
Dr. Galvan holds a Master’s degree in Health Systems Management and a Doctor of Philosophy degree in Nursing science from Texas Woman’s University. Dr. Galvan has been named twice in the Houston Chronicle’s Top 150 Nurses in Houston/Galveston. She is committed to raising awareness about the systemic factors that influence health outcomes and believes in the power of collective action to create a more equitable healthcare system for all.

Emily Hartmann, Executive Director, PHIX
The Role of Health Information Exchanges in Advancing the Integration of NMDOH
Emily Hartmann is the Executive Director at PHIX (Paso Del Norte Health Information Exchange). Under her leadership, PHIX has grown to exchange data with hospitals and clinics across West Texas and Southern New Mexico. Throughout COVID-19, she positioned PHIX as a vital public health resource in El Paso, supporting the Alternative Care Site, COVID-19 testing sites, and mass vaccination efforts with data systems. PHIX continues to collaborate with the community use data to address local challenges, including the integration of clinical and non-medical drivers of health data. Emily also has experience in healthcare analytics and strategy. As a health care consultant at Sg2, she helped hospitals prepare for policy changes and evolving financial models. She also has experience developing health initiatives for the City of Chicago and State of Massachusetts. Hartmann has a Master’s in Public Policy from the Harvard Kennedy School and a Bachelors in Economics from the University of Chicago.

Dr. Kelseanna Hollis-Hansen, Assistant Professor of Public Health, UT Southwestern Medical Center
Sustaining Food is Medicine in the Texas Landscape
Dr. Hollis-Hansen is an Assistant Professor of Public Health at UT Southwestern Medical Center in Dallas, Texas. As Principal Investigator and Director of the Nutrition Initiatives & Community Health Equity lab, Dr. Hollis-Hansen’s work aims to develop effective food retail interventions for areas with limited access to food and identify the impact of food is medicine programs developed with and for people who use food pantries and safety-net health clinics.

Caleb Hill, Director of Integrated Health, Burke
Using Risk Stratification to Identify and Address NMDOH Needs in Rural Communities
Caleb Hill is currently the Director of Integrated Health at Burke, where he coordinates the integration of primary care into the behavioral health setting. Previously, he worked as Project Evaluator on a number of SAMHSA grants. He holds a Master of Public Administration and Bachelor of Arts from Stephen F. Austin State University and is currently pursuing a Master of Science in Computational Social Science from the University of Massachusetts at Amherst.

Angie Hochhalter, Lead Director of Community and Population Health, Aetna Better Health of Texas
Working With Managed Care Organizations to Integrate NMDOH
Angie Hochhalter is Lead Director of Community and Population Health with Aetna Better Health of Texas, where she partners across sectors to address the health of Members and communities. She guides cross-departmental teams to identify and address social determinants of health in ways that mitigate potential risks and amplify individual and community strengths to promote health. She also provides strategic leadership on alternative payment models to address provider and member experience, quality of care, cost, and health outcomes. Angie holds an MBA from Auburn University and a PhD in Cognitive and Biological Psychology from the University of Minnesota.

Dr. Carol Huber, Deputy Chief Public Health and Equity Officer, Institute for Public Health, University Health
What to Expect in the 89th Legislative Session
Dr. Huber is the Deputy Chief Public Health and Equity Officer for University Health. She leads the organization’s Institute for Public Health and champions University Health’s commitment to promoting health, preventing disease, and prolonging life in the Bexar County community through programs, services, and partnerships. Dr. Huber has proven expertise in strategic planning, quality improvement, community health needs assessments, and health informatics in hospital, ambulatory, and managed care environments. She serves as chair of the Texas Value-Based Payment and Quality Improvement Advisory Committee and holds faculty appointments at UT Health Houston School of Public Health and Texas A&M School of Public Health. She has a Bachelor of Science in community health from Texas A&M, a Master of Business Administration from UTSA, and a Doctor of Public Health from UT Health Houston.

Junaid Husain, Chief Executive Officer, Greater Houston Healthconnect
The Role of Health Information Exchanges in Advancing the Integration of NMDOH
Junaid Husain is a 25-year healthcare executive with experience across hospital systems, healthcare services, digital health, medical technology, pharmaceuticals, and biotechnology. His career includes leadership roles in management, finance, operations, business development, and consulting.
As the Acting Chief Executive Officer of Greater Houston Healthconnect—the health information exchange for Southeast Texas—Mr. Husain has built partnerships across thousands of hospitals, health systems, academic medical centers, health plans, and ambulatory practices. Under his leadership, Healthconnect has seen extraordinary growth, expanding its suite of digital health solutions, growing its clinical data repository, and magnifying its financial health—becoming one of the largest and fastest-growing HIEs in the nation.
Mr. Husain’s professional career is a collection of unique experiences and accolades. As an executive for MedData, he led the firm’s Affordable Care Act strategy, spearheading Medicaid expansion efforts across the nation—advocating on behalf of hundreds of hospital systems, thousands of healthcare professionals, and millions of uninsured patients. As a veteran Wall Street healthcare executive, he provided advisory services on billion-dollar healthcare technology investments. As Management Consultant to Fortune-500 pharmaceutical and biotechnology companies, he advised the C-suite on corporate and financial strategy. And finally, as an innovation enthusiast, he has worked for seven startup companies, founded three companies of his own, and serves as an Advisor to several health-tech startups.
Mr. Husain is deeply engaged and committed to public service in our Greater Houston and Texas healthcare communities. He currently sits on the Board of Directors of the Texas Association of Charitable Clinics. He works collaboratively across the Texas Medical Center and beyond, partnering with community stakeholders to advance digital health solutions that improve patient quality, safety, and efficiency of care for all Texans. A thought leader in the community, he regularly speaks on matters pertaining to healthcare, innovation, interoperability, and community impact.
A lifelong learner, Mr. Husain received his BSc from the University of Saskatchewan, MSc from McGill University, and MBA from Queen’s University. In 2010, he received his third Master’s degree—a Master of Liberal Arts from Harvard University—where he was Commencement Speaker for his graduating class.

Hanna Jamal, Vice President of Impact Advisory, Social Finance
Financing the Integration of NMDOH Services into Health Care Delivery
Hanna Jamal is Vice President of Impact Advisory and leads Social Finance’s Texas office. In this role, she helps strengthen the capacity of public and nonprofit partners for more effective and equitable delivery of social services. Her expertise includes designing and managing innovative funding models, including “Pay for Success” and other outcomes-based contracts. Hanna’s work spans a range of focus areas, including health, homelessness, early childhood development, and workforce development.
Prior to joining Social Finance, Hanna worked in international development and disaster relief for various organizations, including Plan International, Acumen, and Doctors Without Borders. Hanna holds an MBA from the McCombs School of Business at the University of Texas at Austin and an MA in Anthropology and Development Studies from the University of Edinburgh in Scotland.

Ken Janda, Professor of Practice in Health Systems Science and Population Health, University of Houston Tilman J. Fertitta Family College of Medicine
Financing the Integration of NMDOH Services into Health Care Delivery
Ken Janda is a Professor of Practice in Health Systems Science and Population Health at the University of Houston Tilman J. Fertitta Family College of Medicine and a Lecturer at Rice University’s Jones Graduate School of Business. He teaches the essentials of health systems, insurance and health care financing to medical and MBA students.
Prior to joining the University of Houston, Ken served for 11 years as President and CEO of Community Health Choice, a nonprofit health insurer that included over 400,000 enrollees in Medicaid, CHIP, and the ACA’s subsidized individual Marketplace. A 40-year veteran of the health industry, Ken previously held executive positions with health insurers Prudential, Aetna and Humana.
Ken is also a warrior for health equity and Founder/Managing Principal of Wild Blue Health Solutions, a Texas-based health care consultancy. Wild Blue focuses on advancing new care and payment models for traditional healthcare and social determinants of health, increasing coverage options, and connecting our most vulnerable populations to health care access. He is passionate about connecting every Texan to quality, affordable care.

Dr. Maninder “Mini” Kahlon, Founder, Factor Health at Dell Medical School
Financing the Integration of NMDOH Services into Health Care Delivery
Dr. Kahlon is the founder of a Texas LLC, that delivers a mental health-first, non-medical approach to chronic condition management. She is also the Director of Factor Health Labs, an academic incubator for programs that address the broader drivers of health in people’s lives. Solutions address conditions such as diabetes, kidney health, maternal health, depression and loneliness, incorporating innovations in the workforce, nutritional and behavioral health science and payment & health systems design. Mini is faculty in the Department of Population Health at Dell Medical School in Austin, Texas, where she was previously a founding Vice Dean. Prior to moving to Texas, she managed the nation’s largest translational science institute at the University of California, San Francisco (UCSF). Mini received her PhD in neuroscience from the University of California, San Francisco (UCSF).

Denise LaRue, Administrative Director, Clinical Integration & Transformation, Harris Health System
Building Capacity for NMDOH Integration through Research Partnerships
Denise LaRue serves as Administrative Director of Clinical Integration and Transformation within Harris Health System’s Population Health platform in Houston, Texas. Her work focuses on building capacity for health equity through initiatives that optimize Harris Health’s ability to focus on disparities, as well as to assess and address health-related social needs within system processes and workflows. These efforts include integrating community resources within health centers, establishing organization-level cross-sector partnerships to improve care across settings, and redesigning care to meet patients’ total health needs. Examples include developing Harris Health’s Food Rx initiatives, establishing a Medical Legal Partnership, and launching the We Ask Because We Care campaign to improve awareness and systematize the collection of quality demographic and social need data among patients. Denise received her undergraduate degree Baylor University and holds a Master’s in Public Health and a Masters in Health Care Transformation, both from the University of Texas.

Raejone Lucas, Wellness Coordinator, Waco Family Medicine
Shared Medical Appointments: An Interdisciplinary Pathway to Reimbursement for NMDOH Services
Rae Lucas is the Wellness Center Coordinator at Waco Family Medicine, holding both a bachelor’s and master’s degree in Exercise Physiology from Baylor University. Rae is an ACSM certified Exercise Physiologist and ACE Certified Group Fitness Instructor.
With a passion for youth fitness, weight loss, and chronic disease management, Rae is committed to making fitness accessible and enjoyable for everyone. She believes in the transformative power of physical activity and works to help her patients and clients find joy in their fitness journeys.
In addition to her role at WFM, Rae coaches part-time at F45 in Waco, where she inspires participants to achieve their personal fitness goals. Outside of her professional endeavors, Rae enjoys cruises, watching football, and spending quality time with friends and family.
Rae’s blend of expertise and genuine enthusiasm for wellness makes her a valuable resource in the community, dedicated to fostering a supportive environment for individuals seeking to enhance their health and well-being.

Carol Luna, Lead Community Health Worker Trainer, AccessHealth
Addressing NMDOH Through a Medical Legal Partnership
Carol Luna has over 6 years of experience working as a Certified Community Health Worker with the Federally Qualified Health Center, AccessHealth. Carol graduated from the Texas School of Business in 2003 as a certified Medical Assistant. She gained her Community Health Worker certification in 2019 from Piney Woods Region Training Center. She currently works with the Population Health Department’s Care Coordination team as the Lead CHW Trainer and Medical Legal Partnership CHW Liaison. The Medical Legal Partnership program works with patients to address civil legal needs identified through Social Determinants of Health screening. Carol is passionate about helping underserved communities in the Greater Houston area through advocacy and community engagement.

Elena M. Marks, Senior Fellow in Health Policy, Rice University’s Baker Institute for Public Policy
Sustaining Food is Medicine in the Texas Landscape
Elena M. Marks, J.D., M.P.H., is the senior fellow in health policy at the Baker Institute. Her work focuses on reforming the $4.5 trillion health system so that it produces positive health outcomes, not just medical services. This work includes incorporating the delivery of and payment for nonmedical interventions into the system when appropriate to improve health outcomes.
Elena has been affiliated with the Baker Institute in a variety of capacities since 2010. Previously, she served as the founding president and CEO of the Episcopal Health Foundation, a $1.3 billion nonprofit, from 2014 to 2022 and as the director of health and environmental policy for the city of Houston from 2004 to 2009. Earlier in her career, she practiced law and started, built and sold a successful law-related business.
Elena holds a bachelor’s degree from Emory University, a law degree from The University of Texas School of Law and a master’s in public health from The University of Texas School of Public Health.

Dr. Charles W. Mathias, Director, Texas Consortium for the Non-Medical Drivers of Health
Opening Remarks
Dr. Mathias is the Director of the Consortium for the Non-Medical Drivers of Health at Rice University’s Baker Institute for Public Policy. With 25 years of experience in behavioral health research, Charles is passionate about addressing the non-medical needs that often accompany health conditions. He understands the critical role that policy plays in creating effective health solutions. He served as a Robert Wood Johnson Foundation Health Policy fellow in Washington, D.C., working on Medicaid policies.

Forest Melton, Health Equity Program Manager, Children’s Health
Practical Strategies for NMDOH Screening and Resource Delivery in Complex Populations
Forest Melton is a Health Equity Program Manager at Children’s Health, where he leads efforts to identify and reduce health disparities within the organization and the broader community. Originally from Phoenix, Arizona, Forest attended the University of Arizona, UT Arlington, and is currently completing his PhD in Clinical Translational Sciences with a minor in Public Health. At Children’s Health in Dallas, where the mission is to “Make life better for children”, Forest oversaw the expansion of SDOH screening into the inpatient and emergency department areas. Additionally, Forest provides strategic direction and direct programmatic support for all health equity initiatives, including working collaboratively to implement targeted interventions to close the equity gap.

Darci Moore, Population Health Programs Coordinator, AccessHealth
Addressing NMDOH Through a Medical Legal Partnership
Darci Moore is an enthusiastic public health professional who works in the Population Health department at AccessHealth. There, she specializes in the supervision and expansion of programs and partnerships that address the barriers patients face relating to their social determinants of health. Darci graduated from the University of Houston with a bachelor’s degree in nutrition and fitness. With her educational background in nutrition, she is a strong supporter of Food as Medicine and other initiatives that address health disparities and ensure that all people have the opportunity for a healthy and enjoyable life.

Dr. Robert Morrow, Executive in Residence, Center for Health Care Data, UT Health Houston School of Public Health
The Role of Health Information Exchanges in Advancing the Integration of NMDOH
Dr. Morrow serves as Associate Professor and Executive in Residence for the UT Health School of Public Health. Before joining the School of Public Health, he served as the market president of Houston and Southeast Texas at Blue Cross and Blue Shield of Texas (BCBSTX). Prior to BCBSTX, Dr. Morrow served as the Director of Medical Quality for the Rural and Community Health Institute of the Texas A&M Health Science Center. His previous career includes being Chief Medical Officer for Memorial Hermann Southwest Hospital in Houston and practicing privately in Family Medicine.
Active in the community, Dr. Morrow is the immediate past Chairman of the Board of the Houston Health Museum and serves on the Boards of Houston Health Connect and Faith in Practice. He was recently on the Board of the Greater Houston Partnership, where he served on the Executive Committee and as Chair of the Healthcare Advisory Committee.
Dr. Morrow’s past service includes the Board of Directors for the Houston Division of the American Heart Association, serving as President for two years. In addition, Dr. Morrow served as Chairman of the Board of the Texas Medical Foundation, Health Quality Institute and as President of the Board of Directors of the Caring For Texas Foundation. Dr. Morrow completed his undergraduate studies at Texas A&M University and received his Medical Degree from McGovern Medical School in Houston, followed by a residency in Family Medicine at Memorial Hermann Hospital Southwest. He also attended the University of Tennessee, where he earned his Master of Business Administration. He is a long-time resident of Sugar Land, Texas, where he still lives with Beth, his wife of 38 years. Together they have two children and 4 grandchildren.

Farin Oldnettle, Care Manager, Burke
Using Risk Stratification to Identify and Address NMDOH Needs in Rural Communities
Farin Oldnettle is currently a Therapist at Burke, where she provides outpatient addiction counseling and behavioral health interventions to high-risk patients. Previously, she interned at Oceans Behavioral Hospital. She is a Licensed Master Social Worker and holds a Master of Social Work and Bachelor of Social Work from Stephen F. Austin State University.

Eliel Oliveira, Chief Executive Officer, Connxus
The Role of Health Information Exchanges in Advancing the Integration of NMDOH
Eliel Oliveira is the CEO of Connxus, the Central Texas Health Information Exchanged based in Austin. Eliel has been a key leader in the development of innovative health information technology in partnership with the Assistant Secretary for Technology Policy and Office of the National Coordinator for Health Information Technology (ASTP/ONC), including a mobile patient engagement platform—with a focus on involving underrepresented populations in the design process—and a community-wide referral management platform that integrates social services referrals, clinical data, and personal needs assessments to support health care providers manage referrals to social services aligned with clinical decisions. He also serves as a Senior Director at the Harvard Pilgrim Health Care Institute (HPHCI) in the Department of Population Medicine at the Harvard Medical School, supporting the FDA Sentinel Operations Center and providing informatics and innovation leadership to the national drug surveillance program (Sentinel).
Prior to joining Connxus, Eliel led the division of Health Informatics in the Department of Population Health at the Dell Medical School at the University of Texas at Austin. Previously, he served as the Chief Information Officer at the Louisiana Public Health Institute (LPHI) in New Orleans, where he led the design and implementation of the Research Action for Health Network (REACHnet) as a Clinical Data Research Network node in the national Patient-Centered Outcomes Research Network (PCORnet). At LPHI, Eliel also provided executive leadership and was a board member of the Greater New Orleans Health Information Exchange (GNOHIE). He previously served as Director of Information Technology for the Louisiana Cancer Research Center and was appointed to support the National Cancer Institute in many biomedical informatics technology design and development initiatives.
Eliel received his Master of Business Administration and a Master of Science in International Development from Tulane University where he also served as an Assistant Professor of Medicine at the Tulane School of Medicine. He is a Fellow of the American Medical Informatics Association and an avid speaker and lecturer on many health informatics topics.

Judy Quisenberry, Executive Director, Valley Baptist Legacy Foundation
Philanthropy’s View of NMDOH
Judy Quisenberry serves as the Executive Director for the Valley Baptist Legacy Foundation in Harlingen, Texas. She has been with the Foundation since its inception in 2011 and initially served as the Foundation’s Grants Director. In this role, she developed the grantmaking program and communication strategy and focused on creating new community partnerships. Judy became Executive Director in 2018 and manages the grantmaking program, which distributes $20 million annually. Valley Baptist Legacy Foundation is focused on improving the health of the residents of the Rio Grande Valley of Texas. She serves on the boards of the Episcopal Church Foundation for the Diocese of West Texas and Texas Rural Funders. Judy has a Master of Business Administration from the University of Texas-Pan American (now UTRGV) and a Bachelor of Business Administration from Southwestern University. She and her husband, Greg, enjoy traveling and spending time with their family at the beach.

Jessica Rios, Director of Health Equity, Community First Health Plan
Working With Managed Care Organizations to Integrate NMDOH
Jessica Rios is the Director of Health Equity with Community First Health Plans. In her role, Jessica is currently working to lead Community First to Health Equity and Health Equity Plus Accreditation. She leads the organization in data collection and creating strategies around removing social barriers for Community First members. Jessica has been with Community First for two years and has received the Healthcare Innovation: 40 under 40.

Dr. Jason Rosenfeld, Associate Professor, UT Health San Antonio
HB1575: Addressing the Non-Medical Needs of Pregnant and Postpartum Patients
Dr. Rosenfeld is a public health professional with over 20 years of experience designing, implementing and evaluating international and domestic community health education and behavior change programs. Jason began his career as a US Peace Corps Volunteer in Ghana. After returning to the US, Jason supported the USAID Food for Peace program before obtaining his Masters in Public Health in Health Education and Behavioral Sciences from the Rollins School of Public Health at Emory University. Since 2011, Dr. Rosenfeld has served as the Director for Global Health at the Charles E. Cheever Jr. Center for Medical Humanities & Ethics at UT Health San Antonio. Jason completed an Executive DrPH in Public Health Leadership through the University of North Carolina’s Gilling’s School of Global Public Health and joined the faculty at UT Health San Antonio in 2019. Dr. Rosenfeld is currently an Associate Professor of Medicine and serves in leadership positions for local, national, and international organizations, including the executive committee of the San Antonio Mayor’s Fitness Council, the Governing Council of the Texas Public Health Association, and member of the Consortium of Universities for Global Health’s Global Operations Committee. Dr. Rosenfeld currently serves as Chief of the Internal Medicine Section for Community Health, Director of the Health Confianza health literacy project, and Director of the South Texas Community Health Worker Workforce Preparedness Collaborative.

Dr. Venessa Schick, Associate Professor of Management, Policy and Community Health, UTHealth Houston School of Public Health
Building Capacity for NMDOH Integration through Research Partnerships
Dr. Schick is a social psychologist and an Associate Professor in the Department of Management, Policy, and Community Health at the UTHealth School of Public Health. Dr. Schick has expertise in community-based research with vulnerable communities and those who serve them, with over 125 publications on the health and wellness of historically disenfranchised individuals. Schick’s research focuses on the needs of vulnerable and underserved populations, including those who have experiences with homelessness, criminal justice involvement, or survival sex work. Much of this work focuses on non-medical drivers of health within these populations, including serving as the Principal Investigator on a clinical trial of homelessness diversion. She is the co-author on several book chapters and co-authored a trade book translated into several languages. Dr. Schick has received multiple awards for her work including the 2013 ‘Outstanding Young Professional Award’ from the American Public Health Association’s Population, Reproductive and Sexual Health Section, and the 2016 Barbara Seaman Award for Activism in Women’s Health ‘Emerging Activist’ award.

Dr. Shreela V. Sharma, Professor of Epidemiology, Founding Director of the Center for Health Equity UTHealth Houston School of Public Health
Sustaining Food is Medicine in the Texas Landscape
Dr. Sharma is Professor of Epidemiology, and founding Director of the Center for Health Equity at the University of Texas School of Public Health in Houston, Texas. Dr. Sharma is a behavioral epidemiologist and a registered dietitian with specific research interest in food and nutrition security and co-occurring social determinants of health, systems science, and health equity and has a robust, federally-funded research program in this area. Dr. Sharma is co-founder of Brighter Bites, a nationwide non-profit dedicated to providing fresh produce and nutrition education to low-income children and their families. She is also co-lead of the Health Equity Collective, a systems coalition to improve care coordination for social determinants of health needs in the Greater Houston region. Dr. Sharma has a PhD in Epidemiology and is a registered dietitian in the state of Texas.

Sara Singleton, Principal, Leavitt Partners LLC
Keynote Address
Sara Singleton is a Principal with Leavitt Partners, a health policy consulting firm based in Washington, D.C. Sara advises a diverse set of clients on federal health care policy issues, including public health, social determinants of health, equity, research and drug development, and the Affordable Care Act.
Prior to her current role, Sara was the Senior Director for Policy and Advocacy at the Cystic Fibrosis Foundation. Sara also served as Deputy Assistant Secretary for Legislation at the US Department of Health and Human Services, where she was the department’s liaison to Congress and as an advisor to the Secretary on legislative matters affecting the department.
Sara has significant experience on Capitol Hill, through her roles as a Policy Advisor with the Senate Health, Education, Labor and Pensions (HELP) Committee under Chairman Tom Harkin from Iowa, as a Legislative Assistant for Senator Richard Durbin from Illinois, and as a Public Health Policy Fellow on the HELP Committee under Chairman Ted Kennedy from Massachusetts. Sara has also held positions in grants management at Harvard Medical School and the National Institutes of Health.

Susan Soto, Staff Attorney, Houston Volunteer Lawyers / AccessHealth Medical-Legal Partnership
Addressing NMDOH Through a Medical Legal Partnership
Susan Soto is a licensed attorney with more than a decade of experience in civil litigation. Prior to earning her law license, Susan was a teacher and principal in Texas public schools for almost 20 years. She has devoted her entire professional life to serving vulnerable communities, and her current role as the Staff Attorney for the Houston Volunteer Lawyers/AccessHealth Medical-Legal Partnership demonstrates her commitment to underserved populations. Susan’s awards include being named one of Houston’s Top Lawyers by H Texas magazine in 2015-2017 and on Houstonia magazine’s Top Lawyers list in 2016-2018. She was named a Super Lawyers Rising Star in 2021. Susan is a member of the Texas Bar College’s Society of Legal Scholars and she is a Fellow of the American Bar Foundation. The American Bar Foundation fellowship is an invitation-only membership limited to legal professionals who demonstrate outstanding dedication to the highest principles of the legal profession and to the welfare of their communities.

Dr. Dimple Sureka, Community Philanthropy Officer, Communities Foundation of Texas
Philanthropy’s View of NMDOH
As a Community Philanthropy Officer at the Communities Foundation of Texas, Dr. Sureka brings her expertise in health and wellness to lead grantmaking across CFT’s health portfolios. Her experience as a researcher and clinician aid in overseeing the broad range of investments, from laboratory research to community-based programming, that fall under her purview. Dimple demonstrates a keen interest in understanding the genetic, environmental, and social factors that contribute to health disparities and potential solutions to overcome them. She believes that addressing the broader umbrella issues of the social determinants of health is integral to achieving health equity and building thriving communities for all.
Dimple received her bachelor’s degree in Evolutionary Biology from Princeton University and subsequently, received her Medical Degree from the University of Texas Health Science Center in San Antonio. She completed her residency in Pediatrics at Washington University in St. Louis and Stanford University School of Medicine. Dimple completed a second residency in Medical Genetics from Stanford University School of Medicine. Dimple was a board-certified Assistant Professor at UT Southwestern, Division of Medical Genetics within the Department of Internal Medicine before deciding to leave clinical practice and pursue other avenues to influence health outcomes.

Rosie Valdez-McStay, Principal, RVM Strategies, Wild Blue Health Solutions
What to Expect in the 89th Legislative Session
Rosie Valadez McStay is a distinguished professional with an impressive track record of over two decades in leadership roles. Following a Congressional Hispanic Caucus Institute fellowship in Washington, DC, Ms. Valadez McStay returned to Texas, where she served as a graduate fellow for the House Public Health Committee at the state capitol. Her journey continued at Texas Children’s Hospital, where she led the System’s health care policy strategy and legislative advocacy as well as the inaugural marketing and outreach division of its managed care organization.
Her impactful collaboration with leading children’s hospitals across the nation resulted in the passage of the Children’s Hospital Graduate Medical Education (CHGME) legislation, a pivotal initiative subsidizing the costs of residency training for the pediatric workforce. At the state level, Ms. Valadez McStay played a crucial role in developing a coalition of health industry, business, and civic leaders to advocate for the passage of the Children’s Health Insurance Program and Medicaid eligibility simplification in Texas. Additionally, she spearheaded the institution’s community health needs assessment process and community benefits program efforts, supporting community-based organizations such as the American Heart Association, the Houston Food Bank, the Greater Houston YMCA, and the Girl Scouts of San Jacinto County.
Driven by a passion for positive impact in the healthcare sector, Rosie Valadez McStay remains dedicated to the well-being of communities through her strategic insights, service, and professional contributions to public health initiatives. As the principal of RVM Strategies, LLC, Rosie leverages her wealth of expertise to guide clients in various facets of healthcare, including business operations, public policy, community health, strategic planning, health care administration, reimbursement, and business development. Specializing in optimizing legislative advocacy with growth strategies, her work focuses on enhancing health partnerships and aligning business efforts with government public policy and funding priorities such as maternal health, Medicaid managed care, and public health programs addressing non-medical drivers of health and health equity.
Rosie holds a Bachelor of Arts in American Studies from the University of Texas at Austin and a Master’s in Public Health from UT Health – Houston. Currently residing in Houston, Texas, she shares her home with her husband, Robert McStay, a successful healthcare attorney and health system executive, their son, Joshua, and their beloved rescue dog, Benny.

Laurie Vanhoose, Principal, Treaty Oak Strategies
Working With Managed Care Organizations to Integrate NMDOH
Laurie Vanhoose is the principal at Treaty Oak Strategies (TOS,) which provides effective strategic counsel on health care policy. Laurie helps her clients navigate the legislature, health and human services, managed care, provider relations, pharmacy and pharmacy benefit managers, and the Medicaid and CHIP programs. Prior to helping found TOS, Laurie was the Director of Policy & Government Programs at the Texas Association of Health Plans, where she worked directly with Texas’ Medicaid managed care health plans to ensure a strong and efficient Medicaid program. Laurie also worked on pharmacy and commercial issues with private payors and Pharmacy Benefit Managers. Prior to joining TAHP, Laurie served as the Director of Medicaid and CHIP Policy at the Texas Health and Human Services Commission, where she directed policy and clinical staff in the design, development, and implementation of Medicaid medical and program policies. Before taking the Director position, Laurie was a Senior Policy Advisor for HHSC and worked on the development of Medicaid Substance Use Disorder services and led the transition of the Medicaid Women’s Health Program to the state-funded Texas Women’s Health Program. Prior to working for the State of Texas, Laurie worked for several advocacy organizations in Texas and Washington, D.C. ensuring access to health care for individuals with disabilities and older Texans.
Laurie has served on Texas’ State Medicaid Managed Care Advisory Committee, Austin Mayor’s Committee for People with Disabilities, Episcopal Health Foundation and Managed Care Social Determinants of Health Learning Collaborative, National Disability Council Developmental Disabilities Advisory Committee, and the Medicaid Evidence-based Decisions Project (MED) at Oregon Health Sciences University.

Megan Villelda, Evaluation Coordinator, Burke
Using Risk Stratification to Identify and Address NMDOH Needs in Rural Communities
Megan Villelda is currently an Evaluation Coordinator at Burke. Previously, she worked as a CNA for a nursing and rehabilitation facility. She holds a Bachelor’s degree in Health Science from Stephen F. Austin State University and is pursuing a Master’s of Public Health at Texas Tech University

Janet Walker, President and CEO, Texas Association of Community Health Plans
What to Expect in the 89th Legislative Session
Janet Walker is the President and CEO of the Texas Association of Community Health Plans. The Texas Association supports its 12 member health plans serving over 2 million people in Texas. The Association engages members to promote quality healthcare and administrative efficiency in healthcare delivery. Before taking her role with TACHP, Janet served as a member of the senior leadership team for SCAN Group and SCAN Health Plan, one of the nation’s leading not-for-profit Medicare Advantage plans, serving more than 270,000 members in California, Arizona, Nevada, New Mexico, and Texas. Janet has a deep understanding of federal and state healthcare law and policy as it relates to value-based care and population health initiatives, serving as senior counsel in her previous role with Crowell & Moring, LLP and as Managing Director of Crowell Health Solutions in Washington, D.C.
Janet has many years of experience working for large health systems and health plans, focusing on managed care and value-based care. In that capacity, she has advised on both the strategic direction and the legal requirements related to health plan operations, Accountable Care Organizations, Bundled Payment Initiatives, Medicare Advantage, and Direct to Employer Contracting, to name a few. Janet also has experience working with insurance departments across the country, including in Texas, Tennessee, Michigan, and Kansas, on many regulatory issues. Janet’s experience also includes handling complex, regulated entity transactions in the wake of increased value-based care joint ventures. Lastly, Janet has extensive experience advising managed care and insurance entities facing challenges from state and federal administrative agencies. Janet received her Juris Doctorate with honors from The University of Texas at Austin in 2005. Janet’s board experience includes Past Board Chair, Board Member, Chair of Audit & Compliance Committee, Mercy Care, Phoenix, Arizona; Past Board Member, Seton Cove / Mandorla, Austin, Texas; Planning Committee The University of Texas Health Law Conference; and Advisory Council, Healthcare Law, and Compliance Institute.

Lisa Wright, President and CEO, Community Health Choice
HB1575: Addressing the Non-Medical Needs of Pregnant and Postpartum Patients
Lisa Wright is the current President and CEO of Community Health Choice (Community), a non-profit managed care organization serving the Greater Houston Area. Lisa has dedicated over 16 years to advancing healthcare access, focusing on providing affordable insurance programs and implementing initiatives that support underserved communities. Under Lisa’s leadership, the organization has achieved record-breaking membership growth and forged impactful partnerships with healthcare providers and community organizations. Recognized by Modern Healthcare as one of 2024’s Top Diversity Leaders in Healthcare, Lisa has also been honored with the 2024 Stevie Award for Woman of the Year in Healthcare and named among the Top 30 Influential Women in Houston.
Prior to her role at Community, Lisa served as a President of Medicare for WellCare, where she directed and led the execution of Medicare business strategies and operational plans for seven states. She also held several positions at United Healthcare and Anthem Blue Cross Blue Shield.
Lisa’s leadership at Community has driven the organization’s growth and diversification leading to significant achievements in addressing social determinants of health. Under her guidance, Community has grown to over 550,000 members, partnered with 25,000 providers and 100 community organizations, and introduced new product lines.
Lisa’s focus on cultural inclusivity, community outreach, and health education has resulted in groundbreaking initiatives that address critical issues such as mental health, food insecurity, and economic empowerment. Her collaboration with the Harris County Public Health Department on the ACCESS Black Maternal Health program provides essential support for healthy pregnancies and safe deliveries, addressing alarming maternal mortality rates among Black women. Additionally, Lisa developed the CareerReady program, a workforce development training program that provides job certifications, tuition support, and pathways out of poverty for expectant mothers and young adults on Medicaid.
Beyond healthcare, Lisa’s impact extends to mentoring and supporting children. She serves on the board of the Boys and Girls Club of Greater Houston as well as Vericel, a company specializing in advanced cell therapies for sports medicine and severe burn care. Lisa’s involvement with her local church community as a Sunday school teacher and her unique perspective as a foster parent further reflect her dedication to service and community.
Lisa completed the Executive Development Program at the Wharton School of the University of Pennsylvania and was invited to participate in management and executive development programs at Centene/WellCare and United Healthcare. She holds a master’s degree in business administration from the University of Maryland and a bachelor’s degree in communication from the University of Kentucky.

Christine Yanas, Vice President of Policy & Advocacy, Methodist Healthcare Ministries
What to Expect in the 89th Legislative Session
Christine Yanas is the Vice President of Policy & Advocacy at Methodist Healthcare Ministries, where she is responsible for the development of the organization’s public health policies and legislative agendas. Chris is an experienced government relations professional with more than 15 years of specialized knowledge and experience in hospital and healthcare public policy. Prior to joining Methodist Healthcare Ministries, Chris served for seven years as the interim CEO and vice president of operations and advocacy at Teaching Hospitals of Texas (THOT) in Austin where she advocated on behalf of the state’s large teaching hospitals. Her career in policy work began at the state capitol as a legislative staffer for a number of rural and urban members of the Texas House of Representatives. A graduate of The University of Texas at Austin, Chris earned a Bachelor of Arts degree with a double major in English and Government.
Hotel Information

Houston Marriott Medical Center
6580 Fannin Street
Houston, TX 77030
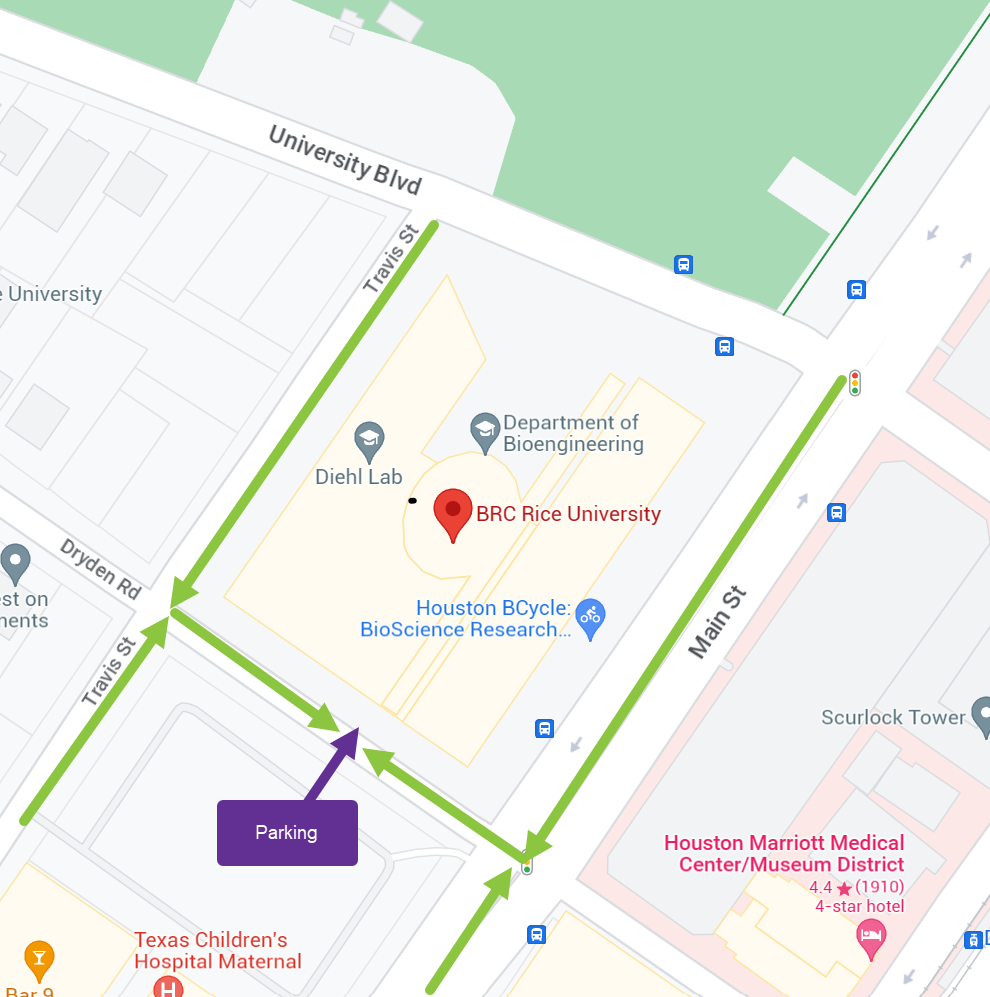
LOCATION & PArking
Rice Bioscience Research Collaborative
6500 Main St
Houston, TX 77030 United States
Parking validations will be provided upon check-in.
Parking garage (BRC Street view)